Concurrent Focal Hepatic and Splenic Lesions: A Pictorial Guide to Differential Diagnosis
Marchelle J. Bean, MD, Karen M. Horton, MD, and Elliot K. Fishman, MD
Abstract: Although medical literature and differential diagnoses discussions tend to be organ specific, systemic diseases more commonly manifest with multi-organ involvement. Detection of dual organ involvement combined with clinical history narrows the differential to provide a more specific diagnosis. Two organs closely linked are the liver and the spleen. Many processes affect both of these organs through their common denominator, the reticuloendothelial system (RES). This pictorial essay reviews the wide spectrum of benign and malignant pathologies to be considered when computed tomography (CT) demonstrates concurrent focal disease in the liver and spleen.
Key Words: liver, spleen, concurrent lesions
(J Comput Assist Tomogr 2004;28:000-000)
Although medical literature and differential diagnosis discussions tend to be organ specific, systemic diseases more commonly manifest with multiorgan involvement. Detection of dual organ involvement combined with clinical history narrows the differential to provide a more specific diagnosis. Two organs closely linked are the liver and the spleen. Many processes affect both of these organs through their common denominator, the reticuloendothelial system. This pictorial essay reviews the wide spectrum of benign and malignant pathologic findings to be considered when computed tomography (CT) demonstrates concurrent focal disease in the liver and spleen.
INFECTIOUS DISEASE
Infectious diseases can spread systemically, resulting in hepatic and splenic abscesses or microabscesses. Presenting symptoms include fevers, chills, abdominal pain, and nausea and vomiting. Abscesses can be bacterial, parasitic, or mycotic and vary in size from a few millimeters to several centimeters.
Widespread disease commonly occurs in immunosuppressed individuals, often because of tuberculosis, histoplasmosis, Pneumocystis carinii, and disseminated bacterial and fungal infections (Figs. 1, 2).
|
|
FIGURE 1. A 52-year-old woman; status after bone marrow transplantation for acute myelogenous leukemia with ringenhancing lesions in the liver and spleen caused by aspergillosis fungal infection.
|
FIGURE 2. A 77-year-old Hispanic woman with cystic hepatic and splenic abscesses caused by echinococcus. This is a rare example without calcification.
Computed tomography demonstrates multiple small areas of low attenuation, often with ring enhancement. Internally, the lesion may mimic a simple cyst or contain septations and debris. The appearance of a host of infectious diseases and metastatic deposits may have an identical imaging appearance, with diagnosis resting on histologic sampling or response to treatment.
Tuberculosis
Tuberculous involvement of the liver and spleen is rare; when present, it is often secondary to primary infection of the lung or gastrointestinal tract. Typical symptoms include high fever, weight loss, and abdominal pain, with jaundice occurring infrequently. Computed tomography findings of hepatosplenic tuberculosis include hepatosplenomegaly and/or multiple, well-defined, round, low-density lesions. Common ancillary findings include abdominal lymphadenopathy and pleural effusions. Although the CT appearance is not pathopneumonic, this does help to support the diagnosis and evaluate the extent of disease.
Ultimately, diagnosis rests on demonstration of acid-fast bacilli in aspirated tissue (Fig. 3).1
Figure 3A |
Figure 3B |
FIGURE 3. A, A 12-year-old boy with tuberculosis. The patient had enlarged low-density mediastinal adenopathy. B, Multiple low-density hepatic and splenic lesions caused by tuberculosis.
Histoplasmosis
The most common granulomatous disease in North America is histoplasmosis. This organism lives in soil containing excrement of bats and birds and is transmitted through inhalation. Primary disease affects the lungs, whereas the disseminated form most commonly involves the liver and spleen. Granulomatous disease produces a specific immune inflammatory response leading to granuloma development. During the active phase of infection, granulomas appear as multiple, small, hypodense lesions, which calcify over time, leaving punctate foci of calcium at sites of previous disease. (Fig. 4).
|
|
FIGURE 4. A 69-year-old woman with multiple calcified granulomas in the liver and spleen, representing a sequela of prior histoplasmosis infection.
Candidiasis
Disseminated candidiasis commonly occurs in immunosuppressed individuals. Computed tomography findings range from multiple, small, low-density hepatosplenic lesions to
hepatosplenomegaly. Punctate calcifications are the sequela of treated disease (Fig. 5).2
|
|
FIGURE 5. A 23-year-old man with a history of acute myelogenous leukemia, who developed candidiasis infection of the liver and spleen. Low-density hepatic and splenic abscesses are present (arrows).
Pneumocystis carinii
P. carinii is a common lung infection in immunocompromised hosts. Extrapulmonary dissemination, although rare, does occur to the liver and spleen. The CT appearance is one of multiple, focal, low-attenuation lesions in the liver and spleen. These lesions become progressively calcified with a rim-like or punctate pattern (Fig. 6).
NEOPLASTIC CONDITIONS
Primary
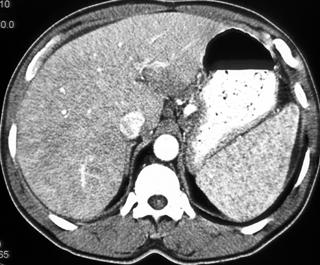
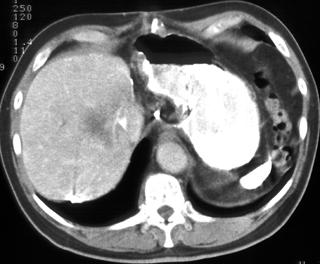
Lymphoma/Leukemia
Lymphoma is a common primary malignancy of the spleen, usually appearing as diffuse homogeneous organ enlargement. Less common forms include a round focal mass or multiple small nodules. Splenic involvement is more common with non-Hodgkin lymphoma than with Hodgkin lymphoma.
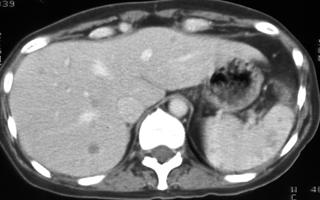
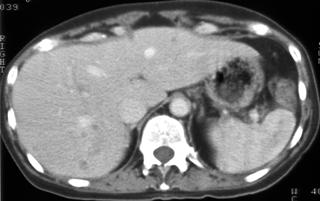
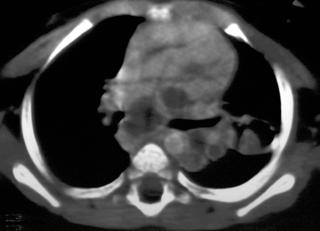
Lymphoma involves the liver in 20%-50% of patients with Hodgkin disease, with a slightly higher rate in non-Hodgkin lymphoma. Hepatic involvement appears as multiple lowattenuation lesions on CT or as diffuse homogeneous involvement producing only hepatomegaly (Fig. 7).
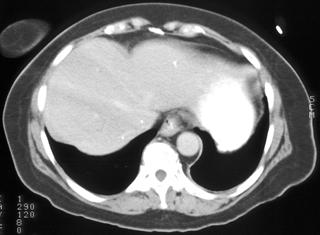
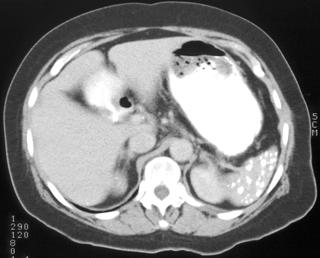
Figure 7A |
Figure 7B |
Figure 7C |
FIGURE 7. A 57-year-old woman with multiple low-density hepatic and splenic lesions (A, B) and abdominal adenopathy (C) caused by lymphoma. There is a difference in linear attenuation through the liver as a result of streak artifact.
Splenic leukemia is more common with chronic forms of the disease, denoting a poorer prognosis and potentially leading to splenic rupture. Leukemia may also involve the liver giving focal nodular lesions.
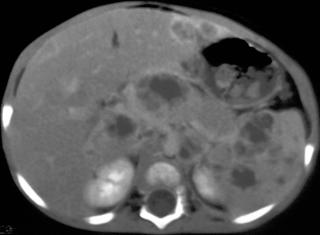
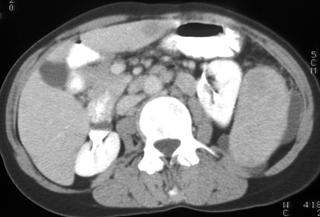
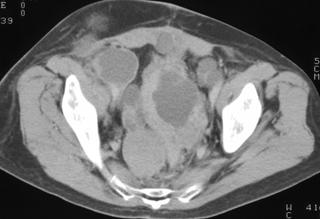
Metastatic Disease
Metastatic disease more often affects the liver than the spleen, despite the spleen's large quantity of lymphoid tissue and filtration of systemic blood flow. Multiple theories have been proposed to explain the spleen's scarcity of metastatic involvement, although none is fully satisfying. Primary tumors commonly associated with hepatic and splenic metastasis include lung cancer, breast cancer, and melanoma (Fig. 8). Hepatic and splenic metastases vary in size from a few millimeters to several centimeters but predominately appear as small hypodense target lesions. The target appearance results from a hypodense center with peripheral ring enhancement. This appearance can easily mimic infectious processes, and differentiation is made through a combination of clinical presentation and histopathologic correlation (Fig. 9).
|
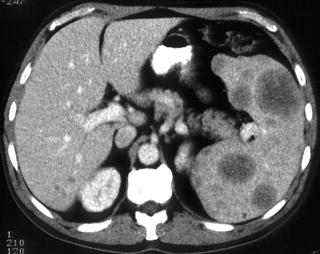
FIGURE 8. A 53-year-old man with metastatic melanoma to the liver and spleen.
Figure 9A |
Figure 9B |
Figure 9C |
FIGURE 9. A 64-year-old woman with metastatic papillary serous ovarian carcinoma; status after total abdominal hysterectomy, bilateral salpingo-oophorectomy, and omentectomy. Innumerable cystic implants are present on the peritoneal surface of the liver and spleen (A, B) as well as throughout the pelvis (C).
MISCELLANEOUS CONDITIONS
Sarcoidosis
Sarcoidosis is a multisystem disease of unknown etiology. Noncaseating granulomas are characteristic of this process and can affect any organ of the body. The lung is most commonly involved (in greater than 90% of sarcoid patients), with resultant typical radiographic manifestations of interstitial lung disease and lymphadenopathy. Other organs, including the skin, eyes, salivary glands, heart, bones, nervous system, and abdomen, are affected less frequently.
Approximately 5%-15% of patients develop abdominal involvement.4,5 Warshauer et al6 showed that abdominal findings relate to clinical status and elevated angiotensinconverting enzyme levels but not to chest radiographic stage. As visualized on CT, the most common abdominal manifestations include hepatomegaly, splenomegaly, and lymphadenopathy. A less common finding is multiple, hypodense, hypovascular, 1-mm to 3-cm hepatic and splenic lesions on CT examination. Nodules tend to be innumerable and variable in size. With coalescence, a diffusely infiltrative appearance with concurrent hepatosplenomegaly may result. Isolated splenic and hepatic lesions are another presentation (Figs. 10, 11).
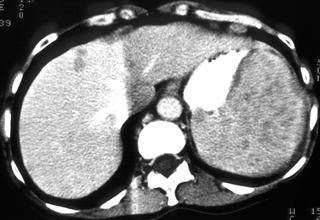
Figure 10 |
FIGURE 10. A 47-year-old woman with multiple low-density lesions of the liver and spleen. Although these lesions were proven to be caused by sarcoidosis, lymphoma could have an identical appearance.
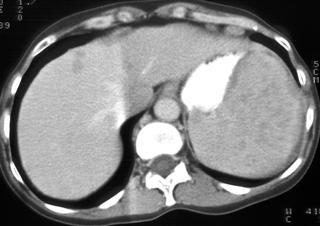
Figure 11A |
Figure 11B |
Figure 11C |
Figure 11D |
FIGURE 11. A 58-year-old man with weight loss, cough, fatigue, and elevated alkaline phosphatase. Computed tomography reveals mediastinal and hilar adenopathy (A), reticular nodular interstitial infiltrates (B), innumerable hepatic and splenic hypodense lesions (C, D), and moderate porta hepatis adenopathy (D) caused by sarcoidosis. The differential diagnosis would include tuberculosis and a neoplastic process.
Amyloidosis
Amyloidosis is a systemic disorder characterized by abnormal extracellular deposition of insoluble fibrillar protein material in almost any organ of the body producing significant morbidity and mortality. Resistant to proteolytic degradation, amyloid replaces and destroys normal tissues in vital organs, such as the heart, kidneys, and gastrointestinal tract, and can be relentless, leading to early and sudden death. Amyloidosis can be primary, with protein deposition caused by excessive secretion from B-cell lymphocytes or plasma cells, or secondary, caused by excess protein deposition as a result of chronic infections and inflammatory processes. These may include but are not limited to tuberculosis, chronic osteomyelitis, rheumatoid arthritis, inflammatory bowel disease, psoriasis, and Hodgkin disease.
Imaging features are nonspecific, mimicking many other diseases. Knowledge of this entity may lead to consideration of this process as a potential diagnosis, however. Microscopy exhibits apple-green birefringence under polarized light after Congo red staining. Amyloidosis of the liver and spleen usually presents with hepatomegaly or splenomegaly. Focal mass lesions consisting of extensive amyloid infiltration are rare.7
Peliosis
Peliosis is an uncommon benign disorder characterized by blood-filled cysts affecting primarily the liver but occasionally the spleen. Other organs potentially involved include the lymph nodes, bone marrow, lungs, pleura, kidneys, adrenal glands, stomach, and ileum. This entity was initially thought to be associated with chronic diseases, including cancer and tuberculosis. Currently, the occurrence of peliosis is reported in patients treated with anabolic steroids and oral contraceptives.
Commonly asymptomatic, this disease may manifest with hepatic failure, portal hypertension, hemorrhage, and hemoperitoneum. Lesions vary in size from 1 mm to several centimeters; they are often hypodense or, less commonly, hyperdense before and after administration of contrast. Lesions are highly variable in imaging appearance, with some enhancing after contrast administration (Fig. 12).8
Figure 12A |
Figure 12B |
FIGURE 12. A 34-year-old woman positive for human immunodeficiency virus presenting with fevers and skin rash. Computed tomography reveals splenomegaly and multiple hypervascular hepatic lesions compatible with peliosis.
Hypereosinophilic Syndrome
Eosinophilia without a demonstrable cause is known as hypereosinophilic syndrome. Initial signs and symptoms are vague and include fever, weight loss, abdominal pain, nonproductive cough, pruritic rash, and congestive heart failure. Diagnostic criteria entail eosinophilia of 1500 eosinophils/mL for longer than 6 months, absence of a definable cause such as allergic or parasitic etiologies, and presence of organ infiltration.
This disease routinely causes hepatosplenomegaly in 85% of individuals because of eosinophilic infiltration of the liver and spleen or passive congestion from the heart. A less common presentation results in focal, hypodense, ill-defined, variably sized hepatic lesions.9
Thorium Dioxide Exposure (Thorotrast)
During the 1940s and 1950s, a radioactive colloid suspension containing thorium dioxide was injected intravenously. This contrast agent, Thorotrast, targeted the reticuloendothelial system, with its uptake giving a high-density appearance to the liver and spleen and permitting better evaluation of these organs. This -emitting compound is long lasting, producing persistent high density of the liver and spleen years later. The long-term radioactivity induces local malignancies as well as bone marrow dyscrasias (Fig. 13).3
Figure 13A |
Figure 13B |
FIGURE 13. A 70-year-old man with hepatoma arising in a region of prior Thorotrast exposure in the liver. High density findings in the spleen and lymph nodes are caused by Thorotrast exposure.
Gaucher Disease
A deficiency of glucerebrosidase leads to accumulation of ceramide in cells of the reticular endothelial system, resulting in Gaucher disease. Clinically, patients have impaired liver function, anemia, and bone pain. Computed tomography findings include hepatosplenomegaly caused by diffuse infiltration of these organs with deposition of ceramide.10 Focal lowdensity lesions in the spleen may develop because of infarction. Ancillary radiographic findings include Erlenmeyer flask deformity of the femur, multiple lytic bone lesions, aseptic necrosis of the femoral head, and generalized osteopenia (Fig.14).
Figure 14 |
FIGURE 14. A 60-year-old man with Gaucher disease. Computed tomography demonstrates characteristic massive splenomegaly. In addition, there are multiple focal splenic lesions and few hepatic lesions, which are less common but reported manifestations of Gaucher disease.
CONCLUSION
Many processes affecting the liver also involve the spleen because of reticuloendothelial system involvement. Combining this knowledge with detection of concurrent hepatic and splenic disease allows the radiologist to streamline a long list of potential diseases, resulting in faster and more efficient diagnosis.
REFERENCES
1. Balsarkar D, Joshi MA. Isolated tuberculous hepatic abscess in a nonimmunocompromised patient. J Postgrad Med. 2000;46:108-109.
2. Shirkhoda A. CT findings in hepatosplenic and renal candidiasis. J Comput Assist Tomogr. 1987;11:795-798.
3. Halpert RD, Goodman P. Gastrointestinal Radiology, The Requisites. St. Louis: Mosby; 1993.
4. Thanos L, Zormpala A, Brountzos E, et al. Nodular hepatic and splenic sarcoidosis in a patient with normal chest radiograph. Eur J Radiol. 2002; 41:10-11.
5. Hoeffel C, Bokemeyer C, Hoeffel JC, et al. CT hepatic and splenic appearances with sarcoidosis. Eur J Radiol. 1996;23:94-96.
6. Warshauer DM, Dumbleton SA, Molina PL, et al. Abdominal CT findings in sarcoidosis: radiologic and clinical correlation. Radiology. 1994;192: 93-98.
7. Friedman S, Henry D. Systemic amyloidosis and the gastrointestinal tract. Gastroenterol Clin. 1998;27.
8. Ferrozzi F, Tognini G, Zuccoli G, et al. Peliosis hepatis with pseudotumoral and hemorrhagic evolution: CT and MR findings. Abdom Imaging. 2001;26:197-199.
9. Kim GB, Kwon JH, Kang DS. Hypereosinophilic syndrome: imaging findings in patients with hepatic involvement. AJR Am J Roentgenol. 1993;161:577-580.
10. Patlas M, Hadas-Halern I, Reinus C, et al. Multiple hypoechoic hepatic lesions in a patient with Gaucher disease. J Ultrasound Med. 2002;21: 1053-1055.